When it comes to skincare concerns, it’s essential to distinguish between different conditions to address them properly. In this article, we will explore the differences between fungal acne and closed comedones, two common skin issues that can often be confused with each other.
By understanding their unique characteristics, causes, and treatment approaches, you’ll be better equipped to identify and tackle these concerns effectively.
Difference between fungal acne vs Comedones
Fungal acne and comedones, such as closed comedones, are two distinct skin conditions with different causes and characteristics. Fungal acne, also known as Malassezia folliculitis, is caused by an overgrowth of the yeast-like fungus called Malassezia on the skin. It appears as small, uniform, red or flesh-colored bumps that are often itchy and can worsen with heat and sweat.
On the other hand, comedones, including closed comedones or whiteheads, are a type of acne lesion caused by the build-up of sebum, dead skin cells, and bacteria within the hair follicles. They appear as small, whitish or flesh-colored bumps and lack inflammation or visible openings. Comedones are typically not itchy unless they become inflamed.
The treatment approaches for these conditions also differ, with antifungal treatments used for fungal acne and topical retinoids, salicylic acid, or benzoyl peroxide used for comedones.
Fungal Acne
Fungal acne, also known as pityrosporum folliculitis, is a type of acne-like condition caused by an overgrowth of a yeast called Malassezia. Despite its name, fungal acne is not actually acne but rather a yeast infection of the hair follicles. It typically appears as small, itchy, red bumps that are often uniform in size and grouped together in clusters.
Fungal acne is more commonly seen on areas of the face like the forehead, hairline, cheeks, and chin. These bumps may worsen with sweat, heat, or humidity. Unlike traditional acne, fungal acne doesn’t involve clogged pores or sebum production. Instead, it occurs due to an overgrowth of Malassezia yeast on the skin.
Causes and Symptoms of Fungal Acne (Malassezia Folliculitis):
Causes of Fungal Acne
Fungal acne, also known as Malassezia folliculitis, is primarily caused by an overgrowth of a type of yeast called Malassezia. Malassezia yeast is naturally present on the skin and is typically harmless. However, certain factors can contribute to its overgrowth, leading to the development of fungal acne. These factors include:
- Humidity and heat: Malassezia yeast thrives in warm and humid environments, which can promote its growth and exacerbate fungal acne.
- Sweating: Excessive sweating can create a moist environment on the skin, providing an ideal breeding ground for Malassezia yeast.
- Occlusive skincare products: The use of occlusive skincare products that trap moisture and block the pores can contribute to the development of fungal acne. These products can include heavy creams, oils, or silicone-based products.
- Weakened skin barrier: Disruptions in the skin’s natural protective barrier can allow the Malassezia yeast to penetrate the hair follicles and cause an infection.
Symptoms of Fungal Acne
Fungal acne typically presents with distinctive symptoms that differentiate it from traditional acne. The following are common symptoms associated with fungal acne:
- Small, uniform bumps: Fungal acne appears as clusters of small bumps on the skin. These bumps are usually similar in size and shape.
- Redness and inflammation: The affected area may exhibit redness, which can be mild to moderate in intensity. In some cases, the bumps may be itchy or cause discomfort.
- Forehead and upper body involvement: Fungal acne commonly occurs on the forehead, hairline, cheeks, chest, and upper back. These areas are more prone to increased sebum production and can provide an optimal environment for the growth of Malassezia yeast.
- Worsening with sweat and heat: Fungal acne tends to worsen with sweating, exposure to heat, and humid conditions. These factors can trigger the yeast overgrowth and exacerbate the symptoms.
- Lack of comedones: Unlike traditional acne, fungal acne does not involve the formation of blackheads or whiteheads (open or closed comedones). Instead, it manifests as small, red bumps without a central pore blockage.
Closed Comedone
Closed comedones, also referred to as whiteheads, are a form of acne characterized by small flesh-colored or white bumps that are slightly raised and usually uniform in size. Closed comedones occur when hair follicles become clogged with a mixture of dead skin cells, sebum (natural oil produced by the skin), and bacteria.
Unlike fungal acne, closed comedones are not associated with a yeast infection. These bumps are typically non-inflammatory and don’t cause redness or itching. Closed comedones are commonly found on areas of the face with higher oil production, such as the forehead, nose, and chin. They may also occur on the chest, back, and shoulders.
Causes and Symptoms of Closed Comedones:
Causes of Closed Comedones
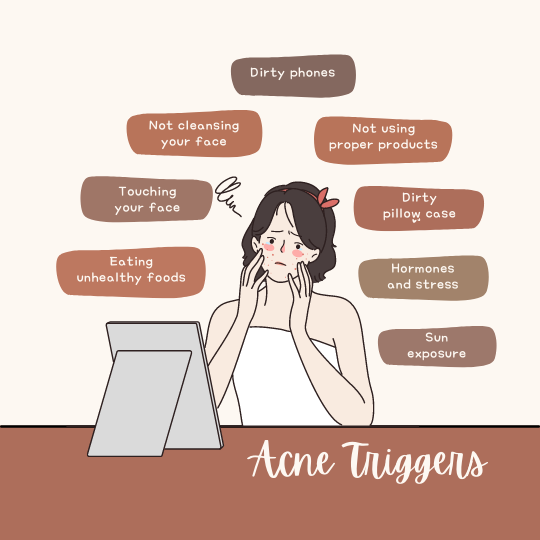
Closed comedones, also known as whiteheads, are a type of acne lesion that occurs when a hair follicle becomes clogged with dead skin cells, oil (sebum), and bacteria. Several factors can contribute to the development of closed comedones:
- Excess sebum production: Overactive sebaceous glands can produce an excess amount of sebum, which can mix with dead skin cells and block the hair follicles, leading to the formation of closed comedones.
- Hormonal changes: Fluctuations in hormone levels, such as during puberty, menstrual cycles, or hormonal imbalances, can increase sebum production and contribute to the formation of closed comedones.
- Cosmetics and skincare products: Certain cosmetic products and skincare formulations that are comedogenic (pore-clogging) can contribute to the development of closed comedones. These products can include heavy creams, oils, or pore-clogging ingredients.
- Genetics: Some individuals may be genetically predisposed to developing closed comedones due to their skin type and the way their sebaceous glands produce and regulate sebum.
- Poor skincare routine: Inadequate cleansing or improper skincare routine can lead to the accumulation of dirt, dead skin cells, and oil on the skin, increasing the risk of closed comedone formation.

Symptoms of Closed Comedones
Closed comedones typically present with specific characteristics that distinguish them from other types of acne. The following are common symptoms associated with closed comedones.
- Small, flesh-colored or whitish bumps: Closed comedones appear as small bumps on the skin’s surface. They are usually flesh-colored or have a white or yellowish appearance.
- Dome-shaped lesions: The bumps have a rounded or dome-shaped appearance and are usually small in size.
- Non-inflammatory: Unlike inflammatory acne lesions, such as papules or pustules, closed comedones are non-inflammatory. They do not exhibit redness, swelling, or tenderness unless they become inflamed or infected.
- Closed pore blockage: Closed comedones occur when the hair follicle opening becomes blocked by a mixture of oil, dead skin cells, and debris. The blockage is not exposed to the air, leading to the characteristic closed appearance.
- Commonly found on the face: Closed comedones typically occur on the face, particularly in areas with a high concentration of oil glands, such as the forehead, nose, and chin (T-zone). They can also appear on the chest, back, and shoulders.
Key Differences between Fungal Acne and Closed Comedone
- Appearance: Fungal acne presents as small, itchy, red bumps that are often uniform in size and grouped together. Closed comedones, on the other hand, appear as flesh-colored or white bumps without inflammation.
- Causes: Fungal acne is caused by an overgrowth of Malassezia yeast, while closed comedones result from the blockage of hair follicles with a mixture of dead skin cells, sebum, and bacteria.
- Symptoms: Fungal acne may be accompanied by itchiness, worsening with sweat and heat. Closed comedones typically do not cause itching or discomfort.
- Location: Fungal acne is commonly seen on the forehead, hairline, cheeks, and chin. Closed comedones tend to appear on areas with higher oil production, such as the forehead, nose, and chin.
Treatment Options
The treatment for fungal acne and closed comedones differs due to their distinct underlying causes.
Fungal Acne Treatment
Fungal acne, caused by an overgrowth of the yeast called Malassezia, requires specific treatment approaches. Here are some options:
- Antifungal Medications: Topical antifungal creams, lotions, or gels containing ingredients like ketoconazole, clotrimazole, or ciclopirox can be applied directly to the affected areas. In severe cases, oral antifungal medications may be prescribed by a dermatologist.
- Antifungal Cleansers: Using antifungal cleansers containing ingredients like selenium sulfide or pyrithione zinc can help reduce fungal growth on the skin. These cleansers are used during showering or bathing and should be left on the skin for a few minutes before rinsing off.
- Avoid Triggers: Identify and avoid triggers that can exacerbate fungal acne, such as excessive sweating, tight clothing, or occlusive skincare products. Keeping the affected areas clean and dry is crucial.
Closed Comedones Treatment
Closed comedones, or whiteheads, require treatment to unclog the hair follicles and prevent further blockage. Here are some options:
- Topical Retinoids: Retinoid creams or gels containing ingredients like tretinoin, adapalene, or tazarotene can effectively treat closed comedonal acne. Retinoids help exfoliate the skin, unclog the follicles, and promote cell turnover. They should be used as directed and may cause initial skin irritation that subsides over time.
- Salicylic Acid: Products containing salicylic acid, such as cleansers, toners, or spot treatments, can help exfoliate the skin, unclog pores, and reduce the formation of closed comedones. Use them according to the instructions provided.
- Chemical Peels: In-office chemical peels performed by a dermatologist can provide deeper exfoliation and help remove closed comedones. Chemical peels use acids like salicylic acid, glycolic acid, or trichloroacetic acid to rejuvenate the skin and improve its texture.
- Extraction: Manual extraction of closed comedones by a dermatologist or esthetician can be an effective method to remove stubborn whiteheads. However, it should be done by a professional to avoid skin damage or infection.
- Skincare Routine: Adopting a consistent skincare routine that includes gentle cleansing, exfoliation, and moisturizing can help prevent closed comedones. Use non-comedogenic products and avoid heavy oils or occlusive ingredients that can clog pores.
Tips to Prevent Fungal Acne and Comedones:
Maintain Good Hygiene
- Cleanse your skin regularly using a gentle, pH-balanced cleanser to remove excess oil, dirt, and sweat.
- Avoid over-cleansing or scrubbing aggressively, as this can irritate the skin and potentially worsen acne or comedones.
Keep the Skin Dry
- Moisture and warmth create an ideal environment for fungal growth. After cleansing or sweating, make sure to thoroughly dry your skin, especially in areas prone to fungal acne, such as the forehead, chest, or back.
- Use a clean towel to pat your skin dry instead of rubbing, as friction can irritate the skin and potentially spread bacteria or fungi.
Avoid Occlusive Products
- Opt for non-comedogenic, oil-free, and lightweight skincare and cosmetic products that won’t clog your pores or trap moisture on the skin’s surface. Look for labels that indicate “non-comedogenic” or “oil-free.”
- Avoid heavy oils, waxes, or emollients that can create a barrier on the skin and contribute to the development of comedones.
Wear Breathable Fabrics
Choose breathable, natural fabrics like cotton or linen for your clothing and bedding. These materials allow better airflow to the skin, reducing the likelihood of sweat build-up and pore blockage.
Avoid Touching or Picking
Refrain from touching or picking at your face, as it can introduce bacteria or fungi to the skin and potentially lead to acne or exacerbate existing conditions like fungal acne or comedones
Practice a Consistent Skincare Routine
Establish a skincare routine that includes gentle cleansing, exfoliation (if appropriate for your skin type), and moisturizing. Consistency is key to maintaining healthy skin and preventing acne or comedones.
PAULA’S CHOICE ANTIOXIDANT PORE PURIFIER
While all the mentioned treatments are effective, we’ll share a personal favorite: Paula’s Choice Antioxidant Pore Purifier. This serum contains salicylic acid, antioxidants, and other beneficial ingredients to address closed comedones.
It helps clear clogged pores, reduce inflammation, and protect against environmental stressors.
This revolutionary product contains an impressive blend of active ingredients like lactic acid and chemical exfoliants that work together to keep malassezia yeast from taking over your skin.
These powerful treatment methods gently remove dirt, oil, and bacteria build-up without drying out your complexion.
Plus, its antioxidant-rich formula defends against free radicals and other environmental aggressors. With regular use of this purifying formula, you’ll notice healthier skin tone and texture that glows with vitality!
Whether you’re looking for a quick fix or a long-term solution to fungal acne issues, Paula’s Choice Antioxidant Pore Purifier has got you covered!
CONCLUSION :Fungal acne vs closed Comedones
In conclusion, fungal acne and closed comedones can be easily confused, as they have similar symptoms. However, the two conditions are quite different: fungal acne is caused by the growth of fungus on the skin, while closed comedones are caused by clogged pores full of dirt and oil.
Fortunately, both conditions can be treated with topical treatments such as Paula’s Choice Antioxidant Pore Purifier. To prevent future breakouts, it’s important to keep your skin clean and moisturized. With a proper skincare routine, you can keep your skin looking healthy and clear!